Psoriasis is an inflammatory skin disease. Occurs when the immune system fails. The development of the disease is divided into clear stages - appearance, progression, stabilization, and regression. Different stages of psoriasis differ in the appearance of spots and rashes, painful itching, and extensive dermatitis.
Why differentiate between the stages of disease development and what are the characteristics of the course of psoriasis at the beginning of development and in the healing process?
Why you need to know the stages of psoriasis
The division of psoriasis into stages is used by physicians to make the right choice of therapeutic methods. The composition of drugs and external agents prescribed to treat inflammation depends on the stage of development of the disease. At the beginning of the onset of the disease, general therapy is needed - vitamin complexes, diet, external aseptic treatment of the rash, such as UV treatments. Also prescribed drugs that stimulate the cleansing of intestines, blood vessels, liver. Be sure to correct the psychoemic condition - neuropathologist or psychologist.
In the early stages of the disease, no strong drugs are used that suppress the immune system, no hormonal ointments are prescribed. These drugs have a large list of side effects, so they should only be prescribed if it is impossible to do without them.
Psoriasis: treatment in acute stages and remission
In the case of an acute progressive disease, several drugs with different effects are prescribed. Immunosuppressants and glucocorticosteroids are often used to relieve inflammation and reduce itching. External treatments are complemented by photochemical, ultrasound and laser therapy. Agents are also prescribed for the antiseptic treatment of damaged skin.
In a stabilized state, they continue to take anti-inflammatory hormonal drugs, gradually reducing their dose. Regenerating ointments are prescribed to repair damaged skin.
In remission - support the body. Proper nutrition, intake of vitamin and mineral complexes to restore immunity.
Timeliness of treatment
The earlier treatment is started, the easier it is to keep psoriasis under control. Timely therapy limits the spread of dermatitis, reduces its extent, and prevents subsequent relapses of exfoliation. Because it is often confused with an allergic rash in the early stages of psoriasis, the initial signs of not missing a skin disease should be known.
Note: Doctors are still investigating the causes of psoriasis. But it is well known that psoriasis dermatitis is not contagious. A patient cannot be admitted and an infection cannot be obtained in the event of an injury. This is our own personal failure in the human body.
Psoriasis is caused by a lack of immunity, which can be caused by a variety of factors. Severe stress, poisoning (including strong drugs, industrial emissions, alcohol), previous infection.
Psoriasis is difficult to treat. The disease is prone to recurrence. And the therapy itself is symptomatic. This consists of preventing the appearance of new spots and relieving existing itchy skin.

Which stage of psoriasis is called initial? How to distinguish between early psoriasis and diathetic rash? And how will the disease develop in the future?
Psoriasis: initial stage
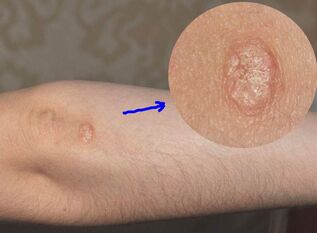
The first appearance of psoriasis on the skin appears to be acne. Most often, the rash appears on the bend of the elbow and knee, or in places where clothing is tight against the body (such as under the waist belt). Rashes can also appear on the edge of the hair and under the hair, around the nails and on the nail plates. Sometimes psoriasis occurs on the legs and palms.
Psoriasis is almost always symmetrical - on the elbows of both hands or on the underside of the back, or on two knees. The pimples themselves (in medical terminology - papules) have a modest appearance in the initial stage. They have:
- Pink or red;
- Sharp, blurred edge;
- Small size - acne on the base does not exceed 2 mm;
- Flat shape - small punctate pimples at the onset of the disease have almost no bulge, so they look mottled.
As the disease progresses, flaky skin flakes appear on the pimples. Gray or silvery, they appear white against a background of red pimples.
The appearance of the balance is associated with severe itching. If it does not resist and is scratched, the scale will be removed and shiny areas of pink, young skin will fall under it. Very thin, vulnerable, itchy papules are scratched for a long time - damaged, bleeding.
The initial stage of psoriasis lasts up to 4 weeks.
Psoriasis: the stage of progression
In the progressive stage, the individual pimples combine into common spots to form what are called psoriatic plaques. They rise above the surface of the skin and are almost completely exfoliated. There is a non-exfoliating pink-red rim on the edge of the psoriasis plaques.
The presence of a rim is a sign of a progressive stage of the disease. The width of the rim is 1-2 mm. The skin on it is inflamed, resembling parchment in structure.
Edge is the expansion area of the spot. This is the skin that is already inflamed but not yet peeling. After a while, the scales also cover it. And the patch expands to cover new areas of skin and form a new wider rim.
With the active development of the disease, the adjacent spots merge with each other. At some point, a large, inflamed red spot may form on the human body.
Psoriasis plaques are very itchy, causing discomfort to the person, disrupting work, rest and sleep. It grows, occupies a large area, and forms a new rash on clean, healthy skin.
The main sign of the progressive stage is the appearance of new rashes. As soon as new pimples and blemishes do not appear, the next stage of psoriasis begins - standing. It’s not a complete victory yet, but it’s already a turn toward recovery.

In the stage of progression, psoriasis is almost always accompanied by weakness, fatigue and weakness. Depression is common. Temperature possible.
The duration of the progressive phase of psoriasis can be long, several months.
Psoriasis: standing stage
The main sign of the stationary section is the disappearance of new spots and rashes. However, the itching also decreases, becoming more tolerable. The rash loses its vivid color, becomes discolored, becomes invisible. This is also a sign of stabilization of the process.
The pink rims around the plaques disappear as the inflammation continues to spread. Active exfoliation and healing begins, the regeneration of new, healthy skin.
It is noticeable to the naked eye that exfoliation increases in the standing phase. The scales completely cover the entire surface of the psoriasis patch, leaving no room for the rims. Psoriasis gets a characteristic flaky appearance that is generally recognized by the population.
Extensive peeling in the standing section is not dangerous. When all the dead cells come off the surface of the psoriasis patch, a light light shade of healthy skin stays in place.
Other signs of progression or stabilization
In addition to the appearance of rash, spots, and scales, there are a number of other signs that can be used to assess the development of the disease. This is the nature of the itching (strong or tolerable), general condition, depressed mood. And the presence of temperature as well.
In the initial stage, the itching is variable, the rash is incomprehensible. Furthermore, the itching increases every day. In the acute stage of psoriasis, it becomes unbearable. It disrupts sleep, rest, disrupts work. The person will be irritable because the itching does not allow for rest.
In the standing section, the itching subsides. Every day - one feels better. The general state of the psyche changes, negativity and depressed moods weaken. The duration of the stationary phase is several weeks - from 2 to 5.
Psoriasis in the attenuation phase
Fading of psoriasis is almost complete disappearance of plaques, spots, redness, inflammation, itching. At this stage of the disease, psoriasis is only reminiscent of different pigmentations of the skin. It appears brighter instead of the former psoriatic spots. The surface of healthy skin has a darker shade.

In some cases, so-called hyperpigmentation develops. In place of psoriasis spots, the skin will not become lighter but darker. In any case, the differences in skin pigmentation will be visible for another month or two.
Psoriasis after recovery: the possibility of relapse
The likelihood of recurrence of psoriasis is determined by a person's lifestyle, diet, allergic mood, and the condition of the body as a whole. It is also determined by the amount of toxins in your body, blood and liver. You can reduce the chance of recurrent dermatitis by strengthening your immune system and cleansing your body of toxins in the liver, blood vessels and intestines.
Seasonal relapses of psoriasis after cleansing are often rare. A person is still susceptible to the disease, but the likelihood of its occurrence is noticeably reduced.
Cleansing the body of toxins and ingesting vitamin and mineral complexes will help boost immunity. This is especially important if immunosuppressants have been used during treatment in the progressive stage of psoriasis. Their need was due to the work of inflammatory mediators. After suppression of autoimmune defense, the immune system must be restored.
Clinical manifestations
Psoriasis is characterized by monomorphic eruptions in the form of papules (lumps) of different sizes, when they fuse together, plaques form and can spread throughout the skin.
At the onset of the disease, in most cases, the rash is limited and forms a single plaque at the sites of your favorite localization (scalp, elongated surface, knee joints, sacrum region, etc. ).
Plaques are clearly demarcated from healthy skin, covered with bright pink or deep red, loose silvery-white scales that can scratch a triad of psoriasis-like phenomena - "stearin stain, " "terminal film, " "blood dew. ". .
Psoriasis has 3 clinical stages: progressive, inpatient, and regressive.
Classification
Depending on the extent of the inflammatory process, the predominant localization of the rash, the severity of the patient's condition and other clinical symptoms, common plaque psoriasis, exudative, arthropathic, pustular, psoriasis erythroderma, psoriasis and psoriasisIt should be noted that different clinical variants may exist in a patient at the same time.
Exudative psoriasis is characterized by a pronounced inflammatory reaction of the skin, manifested by the presence of a lamellar scaly crust on the surface of the plaques, sometimes multilayered, resembling a puff pastry (in which case this form of psoriasis is called a rupioid). When the flaky crust is removed, a weeping surface appears.
Arthropathic psoriasis in the clinical picture, in addition to the usual plaque eruptions, the lesions of the joints are often small, distal, and less frequently large.
Arthropathy can occur in the presence or prevention of skin lesions. Arthritis of psoriasis occurs with pain, swelling, and varying intensity in limiting the mobility of the affected joints, from minor arthralgias in each joint to general lesions and disability in patients. Arthropathic psoriasis is more likely to occur in patients with severe skin rashes (psoriasis erythroderma, pustular psoriasis), but a combination of severe joint damage and relatively limited skin rashes is possible.
Pustular psoriasis can be generalized (Tsumbusha) and limited by involving the palm and soles (Barbera). Stressful situations, infections, irrational general or local therapy contribute to the onset of this severe form of psoriasis.
Generalized in pustular psoriasis with fever, leukocytosis, increased ESR, and general severe condition. Suddenly, small superficial pustules appear in the background of the glossy redness, accompanied by a burning sensation, pain, in the area of ordinary plaques and on previously unchanged skin. New foci of pustulation appear paroxysmal, occupying large areas of skin. The combined pustules cause the epidermis to detach in the form of "purulent ponds, " which can form erythroderma.
Limited pustular psoriasis is more common, with the rash mainly localized on the palms and soles in the form of pustules in the background of erythema and skin infiltration. The course is milder than generalized, with satisfactory general condition, but with persistent, frequent relapses. Irritant topical therapy is a provocative factor.
Psoriasis erythroderma is a severe form of psoriasis that develops with the gradual progression of the psoriasis process and the fusion of plaque elements to the defeat of the whole skin, characterized by sharp hyperemia, edema, skin infiltration abundant large and small lamellar, large lamellae. Subjective - severe itching is often seen. The disease can begin with erythroderma. The general condition worsens (fever, weakness, lymph node reaction, heart failure, impaired liver and kidney function, changes in blood tests, hair loss, etc. ).
Pleated psoriasis is more common in children and the elderly, especially in patients with diabetes. The lesions are found in the armpit, under the mammary glands, in the perineum, inguinal-femoral folds, in the umbilicus, and are characterized by sharp boundaries, saturated red, and mild exfoliation.
Psoriasis of the palms of the hands and soles of the feet may co-exist or coexist with damage to other areas of the skin, characterized by the formation of hyperkeratotic foci and painful cracks covered by scales with clear boundaries. The characteristic psoriasis triad is difficult to recall.
There are three clinical stages of psoriasis
Advanced section. Provocative factors (trauma, psycho-emotional stress, infectious diseases, inappropriate treatment methods, etc. ) can exacerbate the disease with the appearance of abundant small nodules prone to peripheral growth and the formation of plaques of various sizes and contours that can be isolated or large areas of skin universally. occupied until skin lesions.
In the progressive stage, a symptom of an isomorphic reaction (Kebner phenomenon) is characterized by the appearance of even mild, characteristic psoriatic outbreaks at the site of injury.
Stationary section. In the stationary phase, the appearance of new elements ceases and the peripheral growth trend of existing plaques disappears.
Regressive section. The regression stage means a decrease in the intensity of plaque discoloration, flattening, peeling, infiltration, and resorption of elements with the formation of subsequent hypo- or hyperpigmentation foci at the site of previous rashes.
Management
The treatment of psoriasis is aimed at suppressing the proliferation of epithelial cells and eliminating the inflammatory process, taking into account medical history, form, stage, prevalence of the process, associated diseases, age and sex of the patient, specific treatment or medication.
For mild, limited manifestations of psoriasis, topical topical therapy in the form of salicylic ointment, naphthalene preparations, tar or emollient ointment is sufficient. Severe forms of the disease require complex, systemic treatment with detoxification, desensitization, anti-inflammatory drugs of different groups, physiotherapy methods, external drugs, etc. By applying.
This section introduces the most available and state-of-the-art effective methods and tools for psoriasis therapy.
Systemic therapy
There are specificities in the treatment of patients at different stages of the psoriatic process. Treatment of the advanced stage requires special care. During this period, hemodesis is prescribed intravenously drop by drop, 30 percent. 10% sodium thiosulphate solution calcium gluconate solution, at the same time in case of high blood pressure, it is advisable to administer magnesium sulphate solution; emollient creams or 1-2 percent are used externally. salicylic ointment.
Aromatic retinoids.Acitretin (neotigazone) - a representative of the second generation of monoaromatic retinoids for the treatment of severe forms of psoriasis, in a dose of 10-20-30 mg per day, depending on the severity of the skin process. The mechanism of action of acitretin is inhibition of epidermal cell proliferation and normalization of keratinization processes. The drug is particularly effective in combination with PUVA therapy. The teratogenic effect should not be forgotten when prescribing acitretin.
Cytostatics. Methotrexate is used for a long time in the presence of contraindications to psoriasis and other treatments, as a folic acid antagonist, it mainly acts on actively proliferating cells. Very toxic. There are a number of methods of administration, preferably once a week intramuscularly, under strict laboratory control.
Immunosuppressants.Ciclosporin A is prescribed for severe therapeutic psoriasis that is resistant to other therapies. This drug has an immunosuppressive effect, inhibits cell growth processes, inhibits the secretion of activated lymphocytes of cytokines and the expression of interleukin-1 receptors on immunocompetent cells. It is prescribed for psoriasis at a dose of 5 mg / kg body weight per day.
Non-steroidal anti-inflammatory drugsare prescribed for arthropathic psoriasis and to reduce the acute inflammation of exudative psoriasis and erythroderma. Daily drug doses and duration of treatment depend on the intensity of the pain syndrome, the degree of inflammation, and individual tolerance.
The use of systemic corticosteroid drugs in the treatment of psoriasis is inappropriate, leading to the development of torpedo forms of the disease that are resistant to various therapies. In severe arthropathic psoriasis, prolonged intra-articular administration of corticosteroids is possible, the dose and duration of treatment depending on the size of the joint involved and the degree of inflammation.
Physiotherapy treatments.One of the most effective treatments is PUVA therapy or photochemotherapy (PCT). PCT is a combination of long-wave ultraviolet radiation (wavelengths between 320 and 420 nm) and photosensitizing furocoumarin drugs. The use of photosensitizers is due to their ability to increase the sensitivity of the skin to ultraviolet rays and stimulate the formation of melanin. PUVA therapy leads to the inhibition of cell proliferation, the suppression of pathological keratinization, influences the metabolism of prostaglandins and the permeability of cell membranes. The peak of photosensitization occurs 1 to 3 hours after ingestion of 8-methoxypsoralen. The dose of the drug is selected based on the patient's weight. The procedures are issued 3-4 times a week, 20-25 times.
local PCT is also used with external photosensitizers.
The concomitant use of PUVA therapy and retinoids is called Re-PUVA therapy. Severe psoriasis has the greatest clinical effect.
Selective Phototherapy (SFT) - ultraviolet radiation in the medium wavelength spectrum (280-320 nm) without the inclusion of photosensitizers. SFT is used to prescribe PUVA therapy for less pronounced manifestations of the disease, the presence of contraindications.
How to recognize early psoriasis
Treating psoriasis at the earliest stage is most effective. Therefore, it is very important to diagnose in time. Only a dermatologist can tell if you have psoriasis or other skin conditions. However, you can recognize this disease yourself based on a number of characteristic signs:
- Most often, psoriasis first appears on the folds of the arms and legs, on the hair, or where clothing comes in close contact with the body, or rubbed — in the belt of pants, various elastic bands, or straps.
- At the onset of the disease, a very itchy skin rash appears, covered with gray or silvery skin scales that can be removed very easily.
- By removing the scale, thin, shiny and slightly moist skin appears.
- If you scrape the plaque with a similar spatula, removing the scales, blood will appear on the stain as tiny droplets. However, it is better not to use the latter method to self-define psoriasis - it is very easy to get an infection.
For complete confidence, a doctor should be consulted as patients themselves confuse psoriasis with various lichens or allergic dermatitis and use unsuitable medications for treatment.
What to do if you notice symptoms of the initial stage of psoriasis?
Psoriasis cannot be cured once and for all, so the main goal of therapy is to achieve stable and maximum long-term remission. You should know that without proper treatment, psoriasis quickly becomes chronic: exacerbations can occur up to 9 times a year for up to 15 days.
What to do if you suspect you have psoriasis? Often people, after discovering the signs of this disease on their own, make the big mistake of using "heavy artillery" - hormonal ointments (called topical glucocorticosteroids or THCs) without consulting a doctor. Patients usually explain such a move by claiming to have heard from friends that such funds help quickly. This is a big mistake!
What is the danger of such self-healing? Hormonal ointments for psoriasis have many side effects and contraindications. It is highly undesirable to use them without the strict recommendation of doctors about the duration and frequency of use, the area of application on the body, and without considering the individual characteristics of the body.
Non-hormonal agents such as zinc pyrithione should be used to effectively treat early psoriasis. Zinc pyrithione or active zinc is a very effective drug for the treatment of psoriasis, which has a complex effect:
- suppresses the proliferation and inflammation of excess skin cells, reducing scaling and psoriasis plaque formation;
- relieves itching;
- protects damaged skin against bacterial and fungal infections;
- restores the lipid layer and skin’s protective functions.























